Dehydration is a condition that can occur when the loss of body fluids, mostly water, exceeds the amount that is taken in. With dehydration, more water is moving out of individual cells and then out of the body than the amount of water that is taken in through drinking. (Charles Patrick Davis, n.d.)
As you grow up you understand the importance and benefits of drinking plenty of water but as you become older and your bodies change the way they function it gets harder to stay hydrated. It is common for elderly people to get dehydrated and the decrease in kidney function means the hormone that is usually released to stimulate the sense of thirst decreases. Combine this with elderly people living on their own, relying on staff in care environments or suffering from dementia and it’s understandable how this occurs.
Another cause of dehydration is caused from medication. It’s not uncommon for seniors to be on several medications at any given time. Some of these may be diuretic, while others may cause patients to sweat more. (Aplaceformom.com, 2018)
Even mild dehydration adversely affects mental performance and increases feelings of tiredness. Common complications associated with dehydration also include low blood pressure, weakness, dizziness and increased risk of falls. Poorly hydrated individuals are also more likely to develop pressure sores and skin conditions.
Water helps to keep the urinary tract and kidneys healthy and inadequate fluid intake is also one of the most common causes of constipation. (British Nutrition Foundation, n.d.)
What are the symptoms of dehydration?
- Confusion
- Difficulty walking
- Dizziness or headaches
- Dry mouth
- Sunken eyes
- Inability to sweat or produce tears
- Rapid heart rate
- Low blood pressure
- Low urine output
- Constipation
Staying hydrated doesn’t just mean drinking water. If you’re trying to help a loved one or resident at a care home stay hydrated make sure they consume fluids and eat food with a high water content such as fruit, vegetables and soups. A couple of other tips are to try and offer them preferred drinks, try adding lemon or fruits to the water, offer them fluids throughout the day and try and provide a full glass of water with medications.
With reduced sensation of thirst, they may need to be reminded to drink more often. Try keeping a bottle of water next to their chair or bed. Some elderly people will be reluctant to drink because they want to avoid going to the toilet but overall fluid intake does not reduce urinary incontinence frequency or severity. (Nutrition Foundation, n.d.)
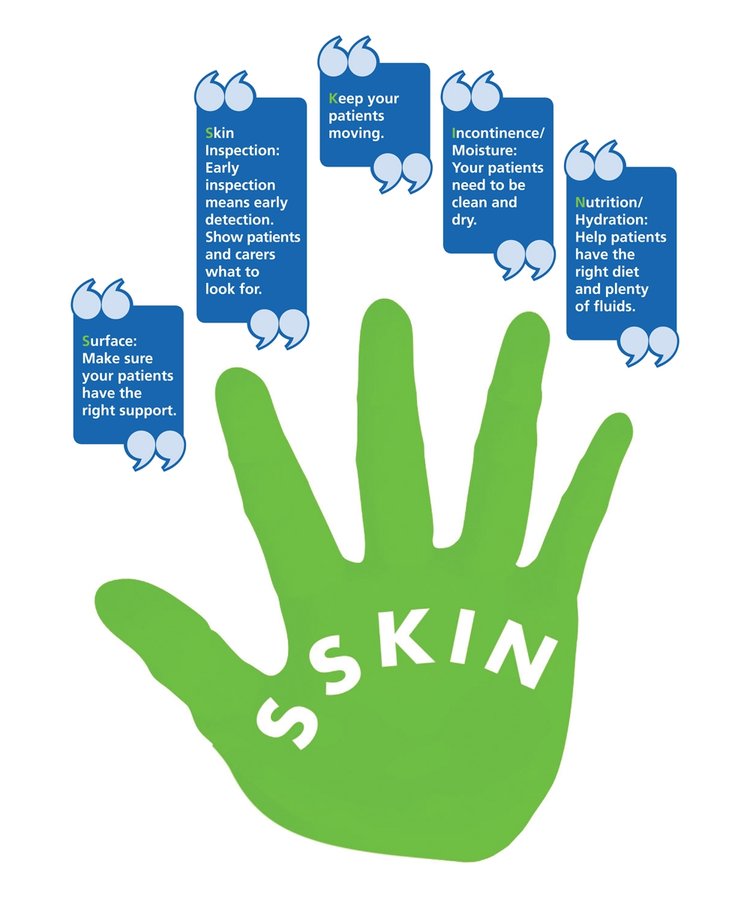
Remember aSSKINg!
As previously mentioned being dehydrated puts you at increased risk or developing a pressure ulcer. The SSKIN model is a five step approach to preventing and treating pressure ulcers. The ‘N’ stands for Nutrition and Hydration and recommends monitoring all food and fluid intake. For more information on the aSSKINg model please contact OSKA’s Clinical Support Nurse, Faith Slater RN. Image source: (NHS, n.d.)
References
Aplaceformom.com. (2018). Elderly Dehydration – A Place for Mom. [online] Available at: https://www.aplaceformom.com/planning-and-advice/articles/elderly-dehydration [Accessed 11 Sep. 2019].
British Nutrition Foundation. (n.d.). Dehydration in the elderly. [online] Available at: https://www.nutrition.org.uk/nutritionscience/life/dehydrationelderly.html [Accessed 11 Sep. 2019].
Charles Patrick Davis, P. (n.d.). Dehydration in Adults Treatment, Causes, Effects & Symptoms. [online] eMedicineHealth. Available at: https://www.emedicinehealth.com/dehydration_in_adults/article_em.htm#dehydration_pictures [Accessed 11 Sep. 2019].
NHS (n.d.). Stop the Pressure. [image] Available at: http://nhs.stopthepressure.co.uk/downloads.html [Accessed 11 Sep. 2019].




